In 2021, more than 170 Australians received a life-saving lung transplant. Bill Van Nierop was one of them.
Bill prepared himself mentally and physically for this precious gift that he received and is incredibly grateful to his donor and their family.
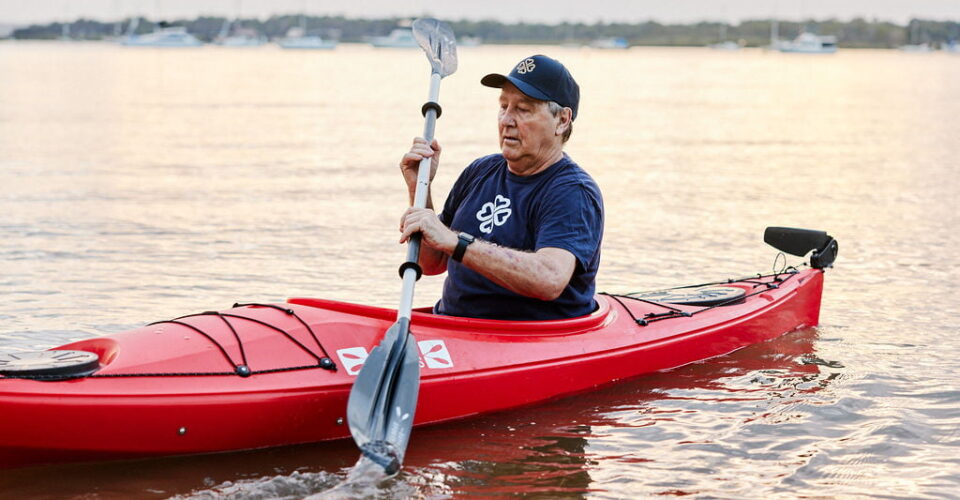
As Bill gets ready to take on the Long Kayak for Lungs 2 – a fundraising feat to raise money and awareness of Idiopathic Pulmonary Fibrosis (IPF) and its impacts – he is bravely sharing his story and opening up about some of the challenges he has faced post-transplant.
Bill says he experiences survivor guilt as some of the patients diagnosed alongside him – many of whom became friends – have not made it this far.
Before we share more about Bill’s life and challenges post-transplant, we talk about the lead-up to a transplant, including what can be an agonising wait for a second chance.
Preparing for a Transplant
Professor Peter Hopkins, Director of the Queensland Lung Transplant Service, says there are several key milestones patients need to meet before they can be deemed eligible for a transplant.
- The first one is, are they medically suitable. We say to patients that it is often not so much about your lung disease, but we want to know if everything else is in working order. So, we replace the car engine, but everything else must be functional for short and long-term survival. Most of the medical testing has little to do with the lungs but more the heart, liver, bone health, vascular health, kidney function etc.
- Secondly, engagement with the team is crucial. Patients and transplant staff must engage well and build trust with each other. It is a two-way relationship. For example, patients have to feel comfortable reaching out and ringing us up after their transplant when they are not feeling well to seek specialist advice.
- And then thirdly, demonstration of broader commitment to exercise, healthy eating, taking medication as prescribed and other lifestyle measures. It is fairly straight forward advice but it is a very demanding schedule that we ask patients to adhere to post transplant, so we must be confident they are able to cope. For example, post-transplant there are potentially up to 30 medications a day to take, a strict exercise program, and dietary changes, including certain food groups we recommend you avoid.
The Difficulty of Waiting for a Life-Saving Transplant
As of July 1, 2023, 108 people in Australia were waiting for a lung transplant.
That wait can be fraught with worry.
“We frequently have patients who ring up and ask if we have forgotten about them, and that is one of the reasons why we see people every four to eight weeks and keep in contact with them,” said Professor Peter Hopkins.
“Sadly, about 20% of our patients die on the waitlist. It is often IPF patients who die waiting because they are deteriorating, and they are quite difficult to match. Their lungs are so small, so getting them a donor is more challenging,” Prof Hopkins added.
Challenges Bill’s experienced so far Post-Transplant
Emotional and Mental Challenges
Bill Van Nierop is incredibly grateful for the life-saving transplant he received. The impact of that gift on the donor and their loved ones is not lost on him.
“I think about a family making that decision at a time of grief and mourning. I’m grateful for that. Really grateful. I just have no comprehension of how they did that but I’m grateful they did,” Bill said.
Sadly, several of Bill’s fellow patients and friends have passed recently. Some were waiting for their own second chance at life, whereas others weren’t considered eligible for a transplant.
“I had a friend diagnosed when I was. We did five clinical trials together, but he didn’t meet the criteria and he didn’t make it to Christmas,” said Bill.
“I said to him one day that I feel guilty. Sometimes I struggle with survivor guilt.”
Along with this emotional toll of his precious gift, Bill speaks about the mental and physical challenges, claiming that many transplant recipients don’t get asked if they’re okay.
“There’s a lot of trauma. For some people, mentally it’s tough. They may angst over the fact somebody died. They angst over the fact that they might get skin cancer. They angst over the fact that they don’t feel well every day. It’s just a different world,” he said.
Bill has also noticed a cognitive decline since his operation and the introduction of new medications.
“I’ve really struggled with my mental side and my mind after the transplant. I was always structured, well planned, and got things done – that was my strength. But in appointments since my transplant, I often get confused with what the medical staff tell me. I find it difficult, and I get more frustrated than I used to,” said Bill.
Physical and Lifestyle Challenges
Transplant patients may face other challenges, including a physically long recovery, an increased risk of skin cancer, adapting to a stringent medication route and transplant rejection.
Professor Hopkins tells patients they have a part-time job to look after themselves after their transplant.
“It’s a very strict schedule taking medications at specific time points. For example, two hours before a meal or one hour after a meal, so you have to plan your day and have alarms set on your phone and other apps that remind you to take the medications when you’re meant to. I say to patients that all the usual health issues we face are even more relevant to them. So it’s important to be vigilant with skin health, bone health, cardiovascular health, because all of these diseases are more common now because you’re immunosuppressed,” Prof Hopkins said, adding that some years the second leading cause of death in the post-transplant population is skin cancer.
“The physical rehabilitation is critical, and we’ve got research that strongly shows if you don’t improve physically in the first few months, you don’t do as well long term. So, building that muscular strength and that endurance is critical after transplant because all lung patients are losing that while they’re waiting because they’re so short of breath.”
“There are structural changes in patient’s muscles and their mitochondria (the energy powerhouse of the cells) as a consequence of their lung disease. And so, they experience muscle atrophy and an energy deficit that needs to be retrained after a transplant.That generally happens with determination and pushing yourself and Bill knows that, so for him, it’s been quite transformational,” said Prof Hopkins.
Professor Hopkins says Bill has negotiated the challenges of his IPF diagnosis and life-post transplant well, describing him as very adaptive.
“I think he’s had a unique ability to be well-informed. I noticed this the first time I met him, he was well-informed, but he also trusted the healthcare provider and was able to assimilate that information with what knowledge he brought to the consultation. And I think that’s very powerful. He would question some of the things that he’d read because there’s a lot of information there and much is just not applicable to the situation you might be facing,” said Prof Hopkins.
“He has very high expectations of himself, which we think is a good thing, and because he trusts us, we’ve been able to tailor his expectations and work his exercise program around what his expectations are, and sometimes maybe lowering them a little bit, but also helping him achieve his goals.”
The Long Kayak for Lungs 2 is Bill’s next goal, and it’s an ambitious one where he will be kayaking about 1200km of the Murrumbidgee River to raise funds for IPF and lung transplant research.
Lung Transplant research supported by The Common Good
The Queensland Lung Transplant Research Service Centre at The Prince Charles Hospital strives to reduce the impact of post-lung transplant disease and lung failure.
These talented researchers are working towards improving transplant recipients’ outcomes and quality of life. Transplant rejection is also a major focus for this research group.
The Common Good and its generous donors support some of this ground-breaking work.
You can read more about their work in our blog here.